Epithelium
- teachanatomy

- Aug 21, 2025
- 15 min read
The human body consists of systems that include the digestive system, respiratory system, urinary system, nervous system and other systems). Body systems comprise organs that have specific forms and functions. Organs consist of different tissues in variable proportions. In turn, tissues are made of cells and cell products arranged in variable forms to give each tissue its characteristic features.

All organs of the body are made of four types of tissue, known as the primary tissues of the body. These are epithelium, connective tissue, muscle tissue and nervous tissue. Each has its own characteristics and specific functions. The different tissues present in any organ work together in harmony to fulfil the specific functions of that organ. If we take stomach for instance, as shown in the illustration above illustration, it contains epithelial tissue, connective tissue, muscle tissue and nervous tissue; this means that it comprises all four primary tissues of the body. The epithelial tissue of the stomach falls into two categories: glandular epithelium and surface epithelium. The glandular epithelium produces gastric digestive enzymes and hydrochloric acid that activates inactive enzymes. The surface epithelium produces large amounts of mucus to protect the stomach wall against the harmful effects of the hydrochloric acid and the gastric digestive enzymes. Muscle tissue present in the wall of the stomach mixes up the food within the gastric lumen and squeeze down towards the intestine. The connective tissue protects and glues other tissues. The nervous tissue controls the functions of other tissues.
Now we shall discuss of the histology of the four primary tissues starting with the epithelial tissue, followed by the connective tissue, then the muscle tissue and finally the nervous tissue.
Epithelial Tissue
Epithelium is a tissue made of closely aggregated cells with minimal amounts of intercellular substance in between. It is avascular - devoid of blood vessels but could be innervated. Epithelial cells usually adhere to each other and rest on a basal lamina. There are different types of epithelia. Epithelial tissues develop from all three germ layers of the developing embryo; some epithelial tissues develop from the ectoderm, others from the mesoderm and some others from the endoderm.
1. Protection of other tissues: Epithelial membrane protects underlying tissues. For example, the tough epithelium that covers the skin is known as the epidermis; it provides a strong protection for the underlying tissues form harmful substances in the surrounding environment (disease causing microorganisms, noxious substances, and harmful rays). Likewise, the lining epithelium of hollow organs and structure of the body protect the delicate underlying tissue form harmful effects of the contents the lumen. Protective epithelial membranes are comparatively thick, may have a layer of keratin and usually adhere to each other by strong intercellular junctions.
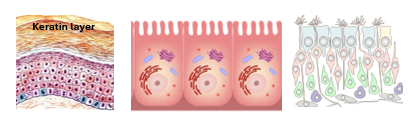
2. Absorption: Some epithelial cells are highly absorptive. For example, cells known as enterocytes present in the lining epithelium of the intestine are highly absorptive. They efficiently absorb nutrients from the lumen of the intestine and pass them to the underlying blood vessels. Such cells are characterized by numerous surface microvilli which are tiny finger-like projections that greatly increase the surface area of absorptive cells. They can be seen clearly with the electron microscope; under the light microscope they appear as apical striations forming what is known as the brush border.
3. Secretion: Secretion is an important function of the epithelial tissue. Some of the epithelial cells are highly specialized in secretion. Secretory epithelial cells could be present in epithelial membranes but are mostly found in gland. They secrete several types of biological molecules including enzymes and hormones. Secretory epithelial cells are equipped with the necessary tools of secretion. They are furnished with organelles (rER and sER) that synthesize the secretory products, and the organelle (Golgi apparatus) that packages the secretory product, and contain the secretory product packaged into secretory vehicles.
4. Sensation: Some epithelial membranes are sensory; they contain sensory cells which act as transducers capable of transforming various types of external signals into electrical nerve impulses that are interpreted by the central nervous system (CNS). In the olfactory region of the nose, the lining epithelium contains sensory cells that detect stimuli generated by odour molecules and send impulses to the CNS. Likewise, sensory cells of the inner ear detect sound waves and produce nerve impulses that can be detected by the CNS.
5. Lubrication: The respiratory passages are lined by a epithelial membrane containing mucous secreting cells known as goblet cells. Mucus is a viscid lubricant. Being part of the mucociliary apparatus, mucus plays an important role in defense against airborne harmful substances (e.g. mucus secreting epithelium of digestive tract. Epithelium of pleura (of the thoracic cavity) and protonium (of the abdominal cavity) produce a lubricant fluid that minimizes friction.
Classification of Epithelial Tissues
Epithelial tissues are classified into two major categories: epithelial membranes and glandular epithelium. Epithelial membranes cover outer surfaces of the body and line surface of body cavities and lumens of hollow organs, whereas glandular epithelium is made of cells specialized in secretion forming glands of various types. Epithelial membranes could be made of a single layer of cells (simple epithelium) or of many layers of cells (stratified epithelium). Glandular epithelium form glands of two major types; exocrine glands passing their sections via ducts to surfaces and endocrine glands which have no ducts and pass their secretions to surrounding tissue fluids and capillaries.

Epithelial Membranes
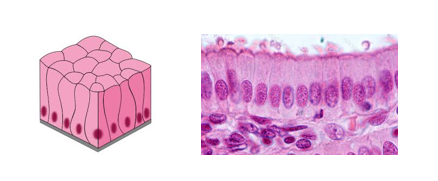
Epithelial membranes are sheets of epithelial cells closely adherent to each other. They are either covering epithelia or lining epithelia. Covering epithelia cover the outer surfaces of the body such as the epidermis of the skin, whereas lining epithelia line inner surface of body cavities such as the thoracic cavity or lumens of hollow organs such as the stomach and intestines or line lumens of hollow structures such as blood vessels. Cells of epithelial membranes have different shapes; they could be squamous, cuboidal or columnar. Squamous cells are thin flat scale-like cells; they have oval nuclei lying parallel to the epithelial surface. Cuboidal cells have equal dimensions (height, width, depth). They could be cubic in shape or polyhedral. They have spherical, centrally located nuclei. They often appear square in sections. Columnar cells are tall column-shaped cells (height greater than width). They have spherical or perpendicularly oriented oval nuclei located in the basal part of the cell. Epithelial membrane cell boundaries are usually indistinct, accordingly histologists rely greatly on nuclear morphology for depiction of epithelial cell shapes. These are the major three forms but there are intermediate forms too.

The Basal Lamina: Epithelial membranes always rest on an amorphous sheet called the basal lamina.it consists of an extracellular matrix composed mostly of glycoproteins secreted by the epithelial cells resting on it. The basal lamina is very thin (<100nm) and can only be seen with the electron microscope; it is very difficult to see with the light microscope except in certain locations (e.g. the glomerular basal lamina in the kidney) utilizing special staining methods. The basal lamina functions as supportive sheet for the overlying epithelial cells, as a barrier between the epithelial membrane and the underlying tissues, and as a selective filter for passage of molecules into and out of the epithelial membrane.
Basement membrane is different from the basal lamina though both are very much related to each other). The basement membrane consists of the basal lamina and reticular fibers (collagen type III).
Simple Epithelia:
Simple epithelia are usually but not always thinner and weaker than stratified epithelia, and thus more permeable and less protective than stratified epithelia. Competent cells of simple epithelia identical to each other. Pseudostratified epithelium is an exception; it is simple but made of dissimilar cells. There are four types of simple epithelium; simple squamous, simple cuboidal, simple columnar and pseudostratified.
Simple Squamous Epithelium: This is the thinnest type of epithelial membranes. It consists of a single layer of thin flat scale-like cells. It has several functions which include:
1. Reduction of friction between adjacent organs or structures.
2. Facilitation of passage of substance across them.
3. Secretion of biologically active substances.
Simple squamous epithelium is common. It is found in the kidney lining Bowman’s capsule and parts of Henle’s loop. It also forms the mesothelium lining the body cavities (peritoneum and pleura), and the endothelium lining the heart, blood vessels and lymphatic vessels. In histological sections examined with the light microscope only the nuclei of the squamous cells are clearly visible,

Simple Cuboidal Epithelium: This type of epithelium consists of a single layer of cube-like cells. All three dimensions of the cell are about the same length. The nucleus is spherical and centrally located. Simple cuboidal epithelium has several functions which include:
1. Secretion
2. Absorption
3. Protection
Simple cuboidal epithelium is also common; it is found in many locations in the body. It found in the thyroid gland where it constitutes the wall of thyroid follicle; it produces the thyroid hormones. It is also found in the kidney forming walls of the proximal and distal tubules of the kidney. Here its main function is absorption. In the proximal tubules, the cells are highly absorptive and show a prominent brush border due to the presence of numerous apical microvilli. Simple cuboidal epithelium is found inducts of some exocrine glands like salivary glands.

Simple Columnar Epithelium: This type of epithelium is made up of a single layer tall cells that resemble short columns. They are characterized by basally located nuclei. The nuclei are either ovoid oriented perpendicular to the basal lamina or spherical in shape. Simple columnar epithelium has several functions which include.
1. Absorption
2. Secretion
3. Protection
Simple columnar epithelium is found in several locations in the body which include.
1. The stomach is lined by a simple columnar epithelium which secretory (mucus), protective and absorptive.
2. The intestinal epithelium is simple columnar with goblet cells (secrete mucus). The columnar epithelia cells are highly absorptive and thus have a striated border (apical microvilli).
3. The gall bladder is lined by highly absorptive and protective simple columnar epithelium.
4. Simple columnar epithelium with or without goblet cells is also present in parts of the ducts of some exocrine glands, such as the parotid salivary gland.
Pseudostratified Columnar Epithelium: Pseudostratified columnar epithelium is a simple epithelium but looks like a stratified epithelium. When looked at with light microscope many layers of nuclei are seen in the epithelial membrane but when examine with the electron microscopes it becomes evident that all cells of the epithelium are resting on the basal lamina, no cell rests on top of another cell. The reason for this unique feature is that the epithelial cells are of different shapes and heights, so their nuclei occupy different levels within the epithelial membrane. The component are usually of three types: a) basal cells which are small short irregular cells with small nuclei occupying the basal parts of the epithelium, b) pyramidal cells which are larger with nuclei occupying the middle parts of the epithelial membrane, c) columnar cells which are tall extending from the basal lamina to the free surface of the epithelium; their nuclei are closest to the free surface of the epithelium. Pseudostratified columnar epithelium is often ciliated and frequently contains goblet cells. Goblet cells are cup-like cells specialized in mucus secretion. The main functions of pseudostratified epithelium are,
1. Protection
2. Secretion
This type of epithelium is a characteristic feature of the respiratory passages from the nose down to bronchi. It is also found in certain parts of the reproductive tract (epididymis an vas deferens).
Cilia and goblet cells of this kind of epithelium participate in forming a strong defensive device called the mucociliary apparatus. Mucus produced by goblet cells participate in forming a sticky mucus blanket that covers the epithelial surface. Airborne harmful particles and organisms are glued to the mucus blanket which is swept towards the pharynx to be swallowed along the glued harmful particles and organisms, ridding the delicate respiratory passage from their adverse effects.

Stratified Epithelia:
Stratified epithelia are epithelial membranes made up of two or more than two layers of epithelial cells. They are usually thicker and more protective than simple epithelia. They are classified into different types according to the shape of cells of the top layer. There are four types of stratified epithelia, these are stratified squamous, stratified cuboidal, stratified columnar and stratified transitional epithelium.
Stratified Squamous Epithelium: This is a common type of epithelial membranes and is one of the thickest. It is a highly protective epithelium; it protects against invasion by harmful organisms, against toxic substances and against dehydration. Stratified squamous epithelia consist of several layers of epithelial cells, with the top layer cells being squamous in shape. Epithelial cells of the other layers are not squamous, they could be columnar, cuboidal or polyhedral. There are two types of stratified squamous epithelium, a keratinized one and non-keratinized one.
1. Stratified squamous non-keratinized epithelium is a thick epithelium. It consists of numerous layers of polymorphic cells topped by a layer of squamous cells. The apical surface is straight whereas the basal surface is wavy. This arrangement strengthens the attachment of the epithelium to the basal lamina and the underlying connective tissue. This type of epithelium lines the oral cavity, the esophagus, the vagina and conjunctiva. The cornea of the eye is covered by a stratified squamous epithelium but is different in that its basal surface in straight and not undulating.

2. Stratified squamous keratinized epithelium is the strongest epithelium, it is dry and constitutes a formidable barrier against harmful organisms and noxious substances. It is quite thick, often being made of more than 10 layers of epithelial cells. It is characterized by the presence of a prominent layer of keratin on top of the epithelial cells. This layer is impervious and waterproof. It is made of dead cells fully packed by a protein called keratin. This type of epithelium constitutes the epidermis of the skin and thus it covers the entire body surface. It poses a mechanical, chemical and immunological barrier against pathogens and harmful substances. The layer of keratin and the strong junctions between the epithelial cells constitute a mechanical barrier. Melanin granules produced by melanocytes and distributed to all epithelial cells constitute a chemical barrier that absorbs UV light and protects against its harmful effects. Immune cells present in the epithelium (Langerhans cells and lymphocytes) constitute an immunological barrier. This type of epithelium often contains sensory nerve endings.

Stratified Cuboidal Epithelium: This type of epithelium is comparatively rare; it is found in some parts of exocrine gland ducts; the ducts of sweat glands and parts of ducts of salivary glands. They are often made of 2-3 layers of cuboidal or polygonal cells.

Stratified Columnar Epithelium: This is type of epithelium always serves two functions, protection and secretion. It is found in parts of the ducts of large exocrine glands. It is often made of two or three layers of polygonal cells overlaid by a row of columnar cells. Goblet cells are sometimes present in-between the columnar cells of the superficial layer.

Stratified transitional Epithelium: This type of epithelium is confined to the urinary passages; for that reason, it is often called urothelium. It is a thick highly protective epithelium. It is quite impervious preventing the underlying tissue from the harmful substances carried by urine. It consists of many layers of epithelial cells that can change their shape in response to external pressure put on them. Thus, a given cell at times appears columnar, at other times cuboidal or squamous. The epithelial free surface may appear wavy when the epithelium is not subject to vertical pressure. When subject to vertical pressure, the epithelium itself appears thinner consisting of flattened cells. This type of epithelium is found in the renal pelvis, ureter and urinary bladder.


Glandular Epithelium
Like epithelial membranes, the glandular epithelium consists of cells closely adherent to each other with a minimal intercellular substance in between. Also, similar epithelial membranes, glandular epithelium is separated from the surrounding tissues by a basal lamina. Glandular epithelium is made up of highly secretory cells that are organized to form different types of glands. Glands are distributed all over the body and are classified by different methods into several different types. Depending on where their secretion passes to, they are classified into two major categories: exocrine glands and endocrine glands.
Exocrine Glands
Exocrine glands pass their secretion on to an external surface (outside the body) or to an internal surface (inside the body) via ducts. Exocrine glands have ducts. They are classified into different types depending on the number of component cells, shape of the secretory units, shape of the ducts and the mode of secretion.
1. Depending on the number of component cells, exocrine glands are classified into unicellular glands and multicellular glands. The unicellular glands are made up of a single secretory cell. Goblet cells are unicellular exocrine glands present within surface epithelial membranes. They produce mucus, have a characteristic cup shaped appearance, and can easily be identified with the light microscope. All other glands are multicellular, made of numerous cells. Some of these multicellular exocrine glands are quite large e.g. the parotid salivary gland, others are minute and can only be seen with the microscope.
2. Secretory units have different shapes, they could be tubular, alveolar, or acinar. In tubular exocrine glands the secretory units take the shape of small tubes. In acinar glands the secretory unit are small pear- shaped with small lumens. Alveolar glands have larger spherical or oval secretory units with wider lumens.
3. Depending on the shape of the excretory ducts, glands are classified into simple glands and compound glands. The ducts of simple glands are not branched, whereas compound glands have branching ducts.
4. Mode of secretion is the method whereby glands pass out their secretion. There are three modes of secretion: merocrine, apocrine and holocrine. Merocrine mode of secretion is the most common mode. Secretion takes place by exocytosis without loss of any part of the cell. Secretory vesicles fuse with the cell membrane and open to exterior of the cell passing their content out of the cell without loss of any part of the cell. Most exocrine glands, e.g. the salivary glands and the exocrine pancreas are merocrine. In the apocrine mode of secretion, the secretory vesicles accumulate in the apex of the secretory cell, which then pinches off from the rest of the cell and passes into the lumen forming the secretion. The secretion is thus made up of debris of the cell apex containing secretory vesicles. The axillary sweat glands are apocrine glands. In the holocrine mode of secretion, the whole cell becomes packed up with secretory vesicles, detached itself from surrounding cells, and passes into the lumen where it disintegrates forming the secretory product. Sebaceous glands of the skin are holocrine.
Exocrine glands are often classified using both the shape of secretory units and shape of the ducts. Thus, glands are described as simple tubular, simple alveolar, simple acinar, compound tubular, compound alveolar or compound tubulo-alveolar. Simple tubular glands have non-branching ducts, and the secretory units are tube-like; intestinal glands are an example of simple tubular glands. Simple acinar glands have non-branching ducts and pear-shaped secretory units; sebaceous glands of the skin are an example. Compound tubular glands have branching ducts and tube-like secretory units; duodenal Brunner’s glands are an example. Compound acinar glands have branching ducts and pear-shaped secretory units; the parotid salivary gland is an example.

Endocrine Glands
Like exocrine glands, the endocrine glands develop in the embryo by invagination of a surface epithelium to the underlying connective tissue. Unlike exocrine glands, they lose connection with the surface and become ductless. Thus, the endocrine cells pass their secretions, which are known as hormones, directly into the surrounding tissue fluids. Hormones secreted into tissue fluids then pass into the blood circulation, to be carried to the targeted cells and tissues.
Endocrine cells are usually present in large groups forming independent endocrine glands such as the pituitary gland. They are also found in groups forming the endocrine component of mixed exocrine and endocrine glands as is the case in the pancreas. In this mixed gland, the endocrine cells form aggregates of cells known as the islets of Langerhans. Endocrine cells are also present scattered diffusely among other nonendocrine cells as is the case with the enteroendocrine cells present in the epithelial membrane of the alimentary tract. Endocrine cell groups usually appear as small cords or ovoid clusters. The arrangement in the thyroid gland is unique; its endocrine cells arrange themselves into small hollow spherical structures known as the thyroid follicles. One other unique feature of the thyroid is that it temporarily stores its hormone outside the cells, in the follicular lumen.
Networks of fenestrated capillaries are always closely associated with endocrine cells to facilitate passage of the hormones from the endocrine cells into the circulation.

Epithelia, Basal Lamina and Cell Junctions.
Epithelial cell groups, whether epithelial membrane or glandular epithelial cells aggregates rest on an amorphous sheet known as the basal lamina., that separates the epithelial tissue form the adjacent connective tissue. The basal lamina is made of laminin and entactin, which are glycoprotein, in addition to collagen, mostly collagen type III. The basal lamina provides support for the epithelial cells. It also acts as a selective barrier.
One other feature of epithelial tissues are the cell junctions that hold the epithelial cells together. They are of different types frequently forming junctional com





Comments